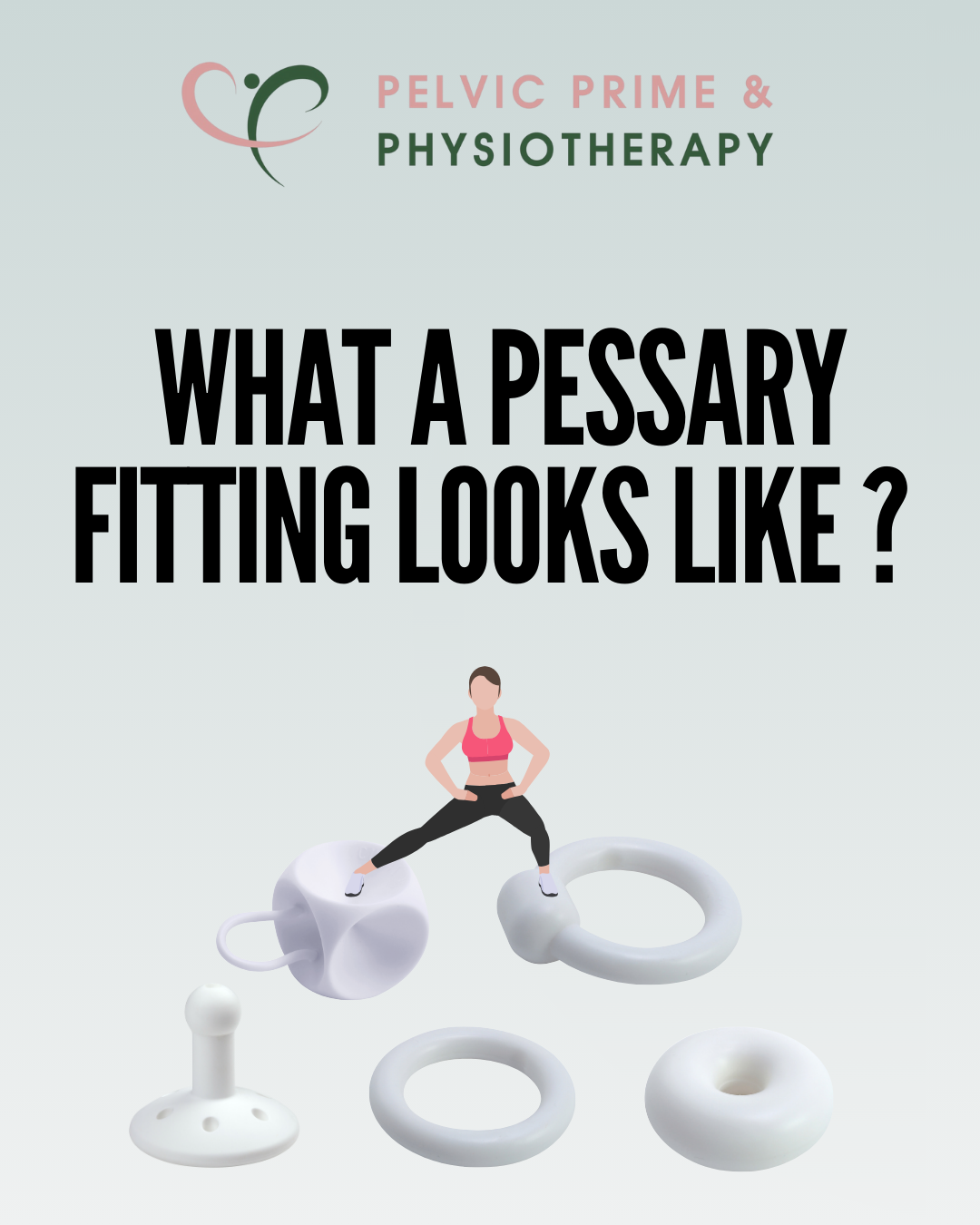
What a Pessary Fitting Looks Like ?

Pessary fitting sounds a bit unfamiliar? Let’s walk through it step by step.
In your initial session, you can talk about your medical history and
prolapse-related symptoms, such as bulging or a ‘coming down’ sensation, heaviness or pressure, urine leakage, constipation, and more.
During the internal exam, your main issues can be identified, such as prolapse, pelvic floor dysfunction, or pelvic floor tightness or weakness.

Once we’ve confirmed that you have stage 2 or 3 prolapse (generally), we will assess whether you are suitable for a pessary fitting.
This includes checking whether you understand how a pessary works, whether you have any contraindications for using a pessary, and whether you’re able to attend regular follow-up appointments

Once you’re considered suitable for a pessary fitting, we’ll obtain your consent.
This includes understanding the possible side effects, agreeing to a vaginal speculum exam, the pessary fitting itself, and regular follow-up check-ups

Before fitting a pessary, we request a vaginal speculum exam from your GP or gynaecologist.
This is an important step to help prevent possible side effects, such as ulceration of the vaginal wall caused by a pessary.
It ensures your vaginal tissue is healthy enough to support the pessary.
It’s also a good opportunity to check whether hormone therapy might be recommended to improve the health of the vaginal wall before the fitting
Afterwards, we determine the right pessary type and size for you, depending on your prolapse and how well your pelvic floor supports it
Once you try a pessary, we make sure it stays in place and feels comfortable in daily life.
We check this with activities like coughing, squatting, or going to the toilet.
If it doesn’t feel right, we try other pessary types until we find the best fit.

You will be trained in pessary self-management—such as how to insert, remove, and clean it, and when it needs to be removed.
We’ll also set up a plan for regular check-ups, usually every 3–6 months after the initial review.
Combining pessary use with regular pelvic floor and core exercises is essential.
This helps strengthen your pelvic floor and can prevent your prolapse from worsening.