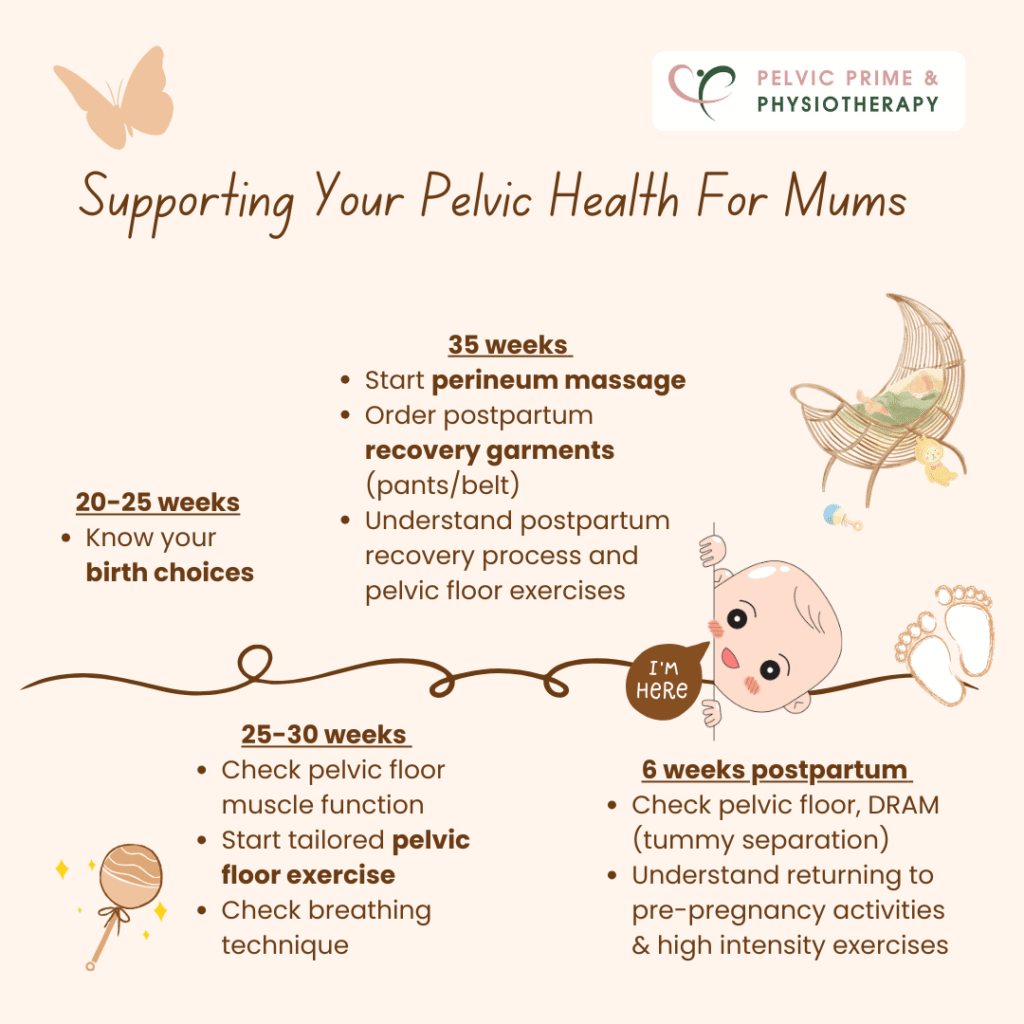
What happens during postpartum period?
The postpartum period is a significant transition for new mothers, both physically and emotionally. One crucial aspect often overlooked is pelvic floor health. After childbirth, many women experience changes in their pelvic floor, which can lead to various issues. This guide will help you understand the importance of pelvic floor management and provide practical tips for recovery.
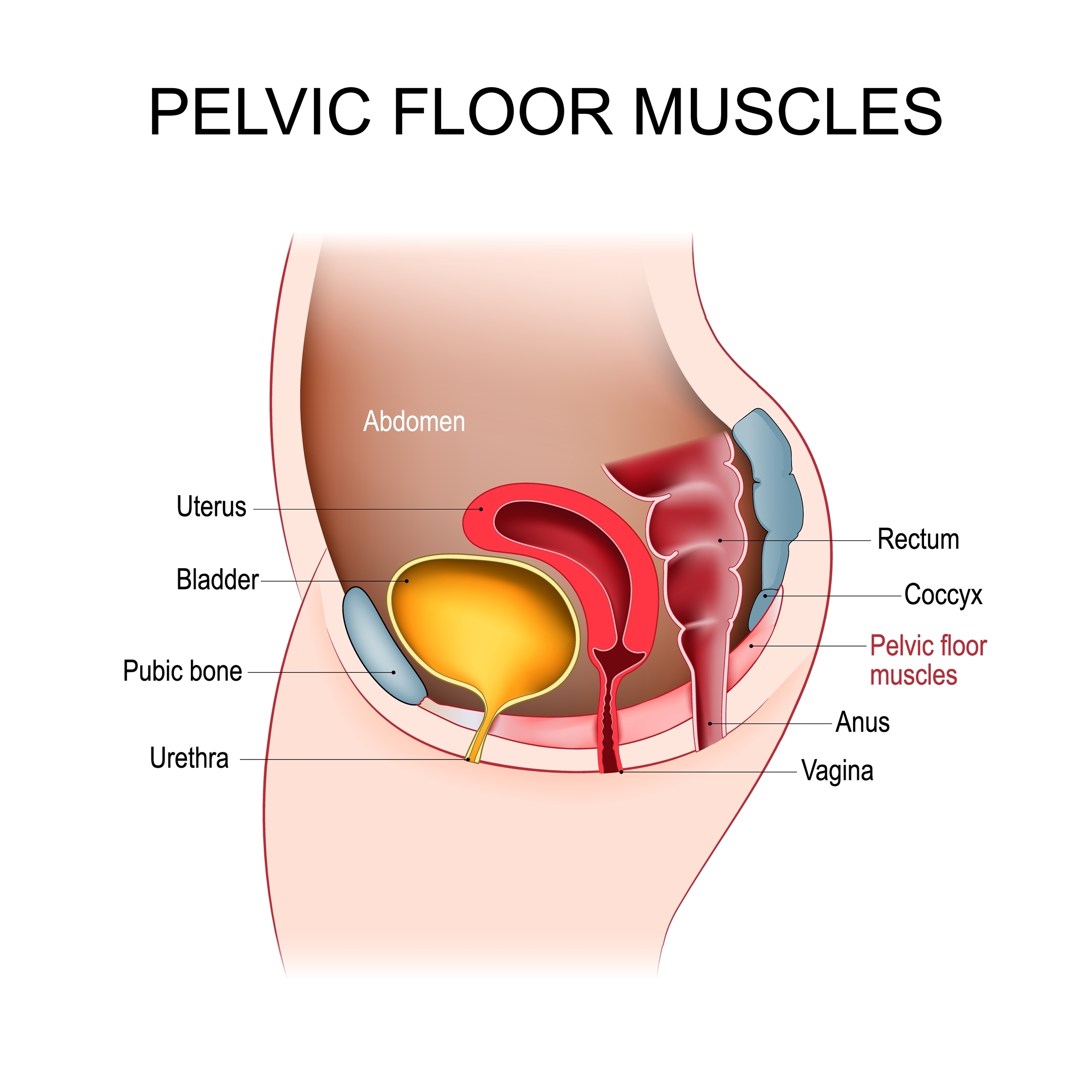
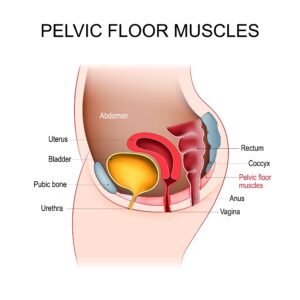
What is Pelvic Floor?
 Pelvic floor is not just muscles in pelvic floor.
Pelvic floor is not just muscles in pelvic floor.
The pelvic floor is a group of muscles, ligaments, and tissues that support the pelvic organs, including the bladder, uterus, and rectum. During pregnancy and childbirth, these structures undergo significant stress and stretching. It’s essential to recognize that postpartum recovery involves restoring strength and function to this area.
Why Pelvic Floor recovery is important during the postpartum period?
 During the pregnancy and delivery, the hormone relaxin increases, causing the pelvic ligaments and muscles to loosen. This prepares the body for childbirth but can also lead to instability in the pelvic area. As the baby grows, additional weight puts pressure on the pelvic floor, stretching and straining the muscles and tissues.
During the pregnancy and delivery, the hormone relaxin increases, causing the pelvic ligaments and muscles to loosen. This prepares the body for childbirth but can also lead to instability in the pelvic area. As the baby grows, additional weight puts pressure on the pelvic floor, stretching and straining the muscles and tissues.
The delivery process can cause trauma to the perineal area, stretching or pulling the ligaments that support the pelvic organs, potentially leading to an avulsion. Additionally, the nerves in the perineum can become damaged or stretched during childbirth.
The common pelvic floor issues after the delivery
Urinary Incontinence
 Urinary incontinence after childbirth can be caused by a combination of physical and hormonal factors related to pregnancy and delivery.
Urinary incontinence after childbirth can be caused by a combination of physical and hormonal factors related to pregnancy and delivery.
Some of the main causes include:
- weakness of pelvic floor muscles,damage to nerve ( damage during labor and delivery,
- particularly from the pressure of the baby’s head on the pelvic nerves or from an epidural) can affect the ability to control urination.
- Hormonal change :After childbirth, hormonal shifts can affect bladder function. For instance, the hormone relaxin, which helps the body prepare for childbirth, can weaken the pelvic floor muscles, making them less effective in supporting the bladder
- Birth Trauma or Tears
Etc.
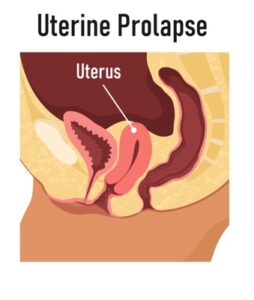
Prolapse

- Post-delivery prolapse occurs when the pelvic organs (such as the bladder, uterus, or rectum) drop or bulge into the vaginal canal
due to weakened pelvic floor muscles. - The symptoms of prolapse after childbirth can vary depending on the severity of the condition and the specific organ involved, but common symptoms include a feeling of heaviness or pressure in the pelvic region and vaginal bulging or a visible lump
- These symptoms may worsen over time, especially in the afternoon or evening
Pelvic Pain

Pelvic pain after delivery can occur for various reasons related to the physical changes and stresses that occur during pregnancy and childbirth.
The symptoms of pelvic pain after delivery can vary in intensity and duration, and can affect different areas of the pelvis.
Localized pain in the Pelvic Area – pain or discomfort in the lower abdomen, near the pubic bone, or between the hips.
This pain can be sharp, aching, or throbbing.
Certain movements, like standing up from a sitting position, walking, or climbing stairs, may aggravate pelvic pain.
This can be caused by muscle strain, ligament relaxation, or residual issues from childbirth.
Sexual pain

Many women experience pain during or after intercourse following childbirth, which may result from vaginal tears, scarring, pelvic floor muscle weakness, or tension.
During vaginal delivery, the perineum (the area between the vagina and anus) may tear or an episiotomy (a surgical cut) may be made to help with the delivery
The muscles of the pelvic floor support the bladder, uterus, and other pelvic organs.
These muscles stretch significantly during delivery, and in some cases, they may weaken or become dysfunctional.
This can lead to vaginal dryness, a feeling of looseness, or even pelvic organ prolapse. Such changes can contribute to pain during intercourse.
After childbirth, hormonal shifts, particularly a decrease in estrogen levels, can affect vaginal lubrication and elasticity.
This can lead to vaginal dryness, making sex uncomfortable or painful. Estrogen levels often take time to return to normal,
particularly if a woman is breastfeeding.
Emotional feeding and emotional issues can cause sexual pain as well
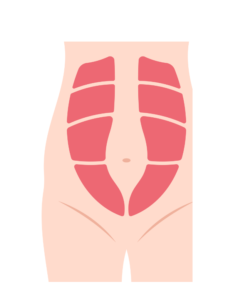
DRAM ( Diastasis)

Diastasis Recti Abdominis (DRAM) means the separation of the two halves of the rectus abdominis muscle, often occurring during or after pregnancy.
Common symptoms include:
- Visible bulge or Pooch
- Weakness or decreased core strength causing back pain or difficulty with movements
- Postural change : DRAM tends to lead to poor posture because the abdominal muscles can no longer provide optimal support for the spine
How Do I know if My pelvic floor is damaged after the delivery?
Assessment with a Pelvic Floor Physical Therapist: A specialized therapist can perform a thorough assessment, including an internal exam if appropriate. They will evaluate muscle tone, strength, endurance and coordination.
Self Assessment : check if you have urinary incontinence symptoms. especially with physical activities which give you strong pressure on lower abdomen like laughing, jumping and running. Check if you have heaviness or discomfort or pain on your perineum area.
How long does it take for the pelvic floor recovery?
We generally expect that six weeks postpartum is the right time for recovery following delivery. Most women can regain normal pelvic floor function after injuries related to childbirth. However, recovery can vary depending on factors such as the conditions of the pregnancy, the type of delivery, and any trauma experienced during pregnancy and deliver.
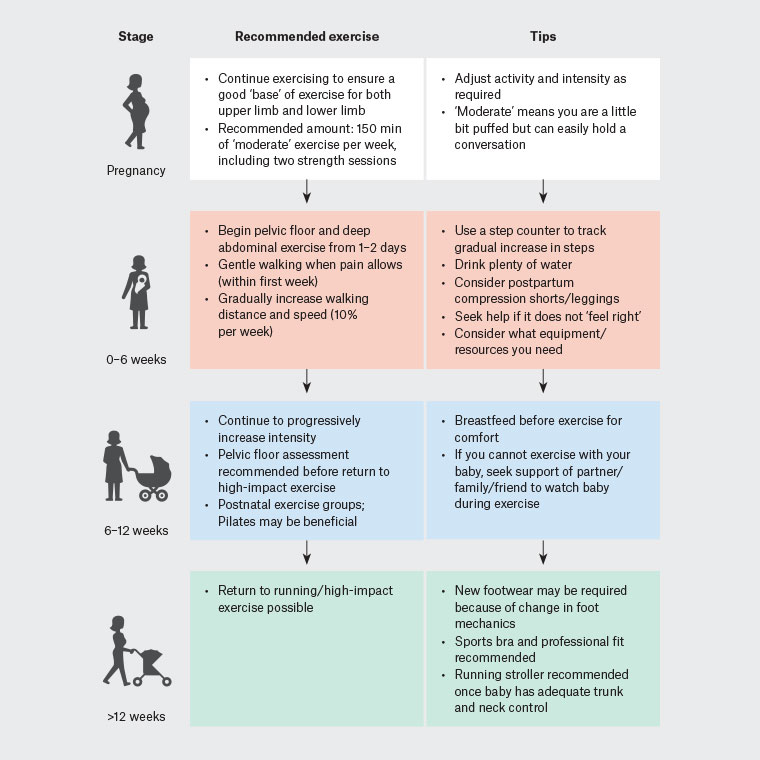
What kinds of exercise will be helpful for pelvic floor recovery?

(Source : Return to exercise post pregnancy, Philipp Inge Jessica J Orchard Rosie Purdue John W Orchard, 2022), doi: 10.31128/AJGP-09-21-6181
Link :Exercise after pregnancy (RACGP)
https://www1.racgp.org.au/ajgp/2022/march/exercise-after-pregnancy










 The symptoms are vary : some has occasional dribbles, some has complete loss of bladder control, resulting in fully wetting their pants.
The symptoms are vary : some has occasional dribbles, some has complete loss of bladder control, resulting in fully wetting their pants.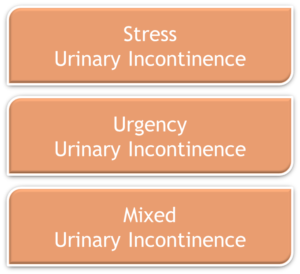 Involuntary loss of urine during physical activities that put pressure on the bladder
Involuntary loss of urine during physical activities that put pressure on the bladder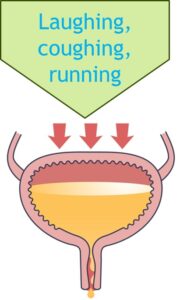 Involuntary loss of urine during physical activities that put pressure on the bladder, such as coughing, laughing, or running.
Involuntary loss of urine during physical activities that put pressure on the bladder, such as coughing, laughing, or running.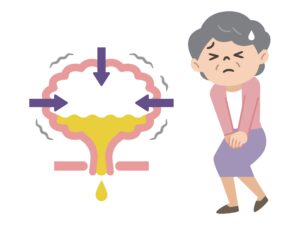 Involuntary loss of urine associated with urgency
Involuntary loss of urine associated with urgency When a person is unaware of the leakage until it has already occurred
When a person is unaware of the leakage until it has already occurred